Connect With Us
Blog
Items filtered by date: July 2024
Preventing Foot Blisters

Preventing blisters is key to maintaining foot comfort, especially for active individuals. Symptoms often include a painful, fluid-filled sac on the skin caused by friction or ill-fitting footwear. To avoid blisters, choose shoes that fit well and break them in gradually. Moisture-wicking socks and blister prevention products like moleskin or blister pads can reduce friction. If a blister does develop, resist the urge to pop it as it can increase the risk of infection. Instead, keep it clean and covered with a bandage. For pain relief, over-the-counter creams or pain relievers can help. Persistent or severe blisters may require attention from a podiatrist, who can provide expert care and guidance. They can recommend appropriate footwear, assess underlying causes, and offer treatments like draining the blister safely to promote healing and prevent complications. If you suffer from blisters, it is suggested you make an appointment with a podiatrist for a treatment plan.
Blisters may appear as a single bubble or in a cluster. They can cause a lot of pain and may be filled with pus, blood, or watery serum. If your feet are hurting, contact David Mehl, DPM of New York. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters are often the result of friction. This happens due to the constant rubbing from shoes, which can lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
Symptoms
(Blister symptoms may vary depending on what is causing them)
- Bubble of skin filled with fluid
- Redness
- Moderate to severe pain
- Itching
Prevention & Treatment
In order to prevent blisters, you should be sure to wear comfortable shoes with socks that cushion your feet and absorb sweat. Breaking a blister open may increase your chances of developing an infection. However, if your blister breaks, you should wash the area with soap and water immediately and then apply a bandage to the affected area. If your blisters cause severe pain it is important that you call your podiatrist right away.
If you have any questions, please feel free to contact our offices located in Forest Hills, and Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Understanding and Managing Plantar Fasciitis
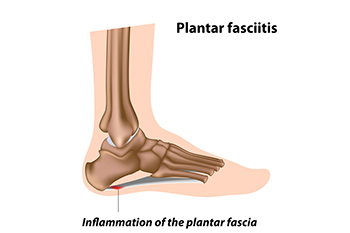
Plantar fasciitis is an inflammation of the plantar fascia, the thick band of tissue along the bottom of the foot, connecting the heel to the toes. Symptoms can include sharp heel pain, especially with the first steps in the morning or after long periods of rest. Diagnosis is typically based on a physical examination and patient history, sometimes supplemented by imaging tests. Relief tactics involve a combination of rest, stretching exercises, and proper footwear with good arch support. For persistent cases, orthotic devices or medical interventions such as corticosteroid injections may be necessary. Early and consistent treatment is key to alleviating symptoms of plantar fasciitis and preventing chronic discomfort. If you have heel pain, it is strongly suggested that you promptly contact a podiatrist who can accurately diagnose the problem, and treat it accordingly.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact David Mehl, DPM from New York. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions, please feel free to contact our offices located in Forest Hills, and Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Prevent Athlete’s Foot
 Tinea, or fungal foot infections, commonly known as athlete's foot, occur when fungi thrive in warm, moist environments, such as between the toes. These infections are extremely contagious, spreading through direct contact with infected skin or surfaces like locker room floors and swimming pools. Individuals at a higher risk include athletes, those with compromised immune systems, and people who frequently wear tight, non-breathable footwear. Symptoms include itching, burning, and peeling skin, often accompanied by redness and blisters. To prevent tinea, it is important to keep feet clean and dry, especially between the toes. It is helpful to wear breathable shoes and moisture-wicking socks, change socks regularly, and use antifungal powders. Avoid walking barefoot in public places and ensure shoes fit properly to reduce risk. In persistent cases, prescription medications may be necessary. If you have developed athlete's foot, it is strongly suggested that you visit a podiatrist for proper management.
Tinea, or fungal foot infections, commonly known as athlete's foot, occur when fungi thrive in warm, moist environments, such as between the toes. These infections are extremely contagious, spreading through direct contact with infected skin or surfaces like locker room floors and swimming pools. Individuals at a higher risk include athletes, those with compromised immune systems, and people who frequently wear tight, non-breathable footwear. Symptoms include itching, burning, and peeling skin, often accompanied by redness and blisters. To prevent tinea, it is important to keep feet clean and dry, especially between the toes. It is helpful to wear breathable shoes and moisture-wicking socks, change socks regularly, and use antifungal powders. Avoid walking barefoot in public places and ensure shoes fit properly to reduce risk. In persistent cases, prescription medications may be necessary. If you have developed athlete's foot, it is strongly suggested that you visit a podiatrist for proper management.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with David Mehl, DPM from New York. Our doctor will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our offices located in Forest Hills, and Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Key Strategies for Preventing Gout
 Gout, a painful form of arthritis that often affects the big toe, can be prevented through lifestyle and dietary changes. Maintaining a healthy weight also reduces the pain of gout by decreasing the stress on joints. Eating a balanced diet that limits purine-rich foods, such as red meat, shellfish, and sugary beverages, helps lower uric acid levels. Staying well-hydrated by drinking plenty of water aids in flushing out excess uric acid from the body. Regular physical activity not only supports weight management but also improves overall joint health. Limiting alcohol consumption, especially beer, can help prevent gout flare-ups. Additionally, managing medical conditions like hypertension and diabetes effectively reduces the risk. For those with a history of gout, regular check-ups and prescribed medications can help maintain lower uric acid levels. Gout in the big toe can cause severe pain and discomfort. If you are experiencing gout attacks, it is suggested that you are under the care of a podiatrist who can help you manage this condition.
Gout, a painful form of arthritis that often affects the big toe, can be prevented through lifestyle and dietary changes. Maintaining a healthy weight also reduces the pain of gout by decreasing the stress on joints. Eating a balanced diet that limits purine-rich foods, such as red meat, shellfish, and sugary beverages, helps lower uric acid levels. Staying well-hydrated by drinking plenty of water aids in flushing out excess uric acid from the body. Regular physical activity not only supports weight management but also improves overall joint health. Limiting alcohol consumption, especially beer, can help prevent gout flare-ups. Additionally, managing medical conditions like hypertension and diabetes effectively reduces the risk. For those with a history of gout, regular check-ups and prescribed medications can help maintain lower uric acid levels. Gout in the big toe can cause severe pain and discomfort. If you are experiencing gout attacks, it is suggested that you are under the care of a podiatrist who can help you manage this condition.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact David Mehl, DPM from New York. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions, please feel free to contact our offices located in Forest Hills, and Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What are Pressure Ulcers on the Feet and Ankles?
 Pressure ulcers on the feet and ankles, also known as pressure sores or bedsores, are injuries to the skin and underlying tissue resulting from prolonged pressure. These ulcers are common in individuals with limited mobility, and can often affect the feet. Intrinsic factors, such as poor nutrition, age, and medical conditions like diabetes, affect the body's ability to heal and withstand pressure. Extrinsic factors involve external forces like friction and prolonged pressure from staying in one position. Symptoms include redness, pain, and open sores, which can progress to deep wounds exposing muscle and bone. Pressure ulcers occur due to reduced blood flow to the affected area, leading to tissue damage. Prevention includes regularly changing positions, using supportive devices, maintaining good nutrition, and keeping the skin clean and dry. Treatment involves relieving pressure, cleaning wounds, and using dressings or medications to promote healing. Advanced cases might require surgical intervention. If you are suffering from a pressure ulcer on your feet or ankles, it is suggested that you schedule an appointment with a podiatrist as soon as possible for care.
Pressure ulcers on the feet and ankles, also known as pressure sores or bedsores, are injuries to the skin and underlying tissue resulting from prolonged pressure. These ulcers are common in individuals with limited mobility, and can often affect the feet. Intrinsic factors, such as poor nutrition, age, and medical conditions like diabetes, affect the body's ability to heal and withstand pressure. Extrinsic factors involve external forces like friction and prolonged pressure from staying in one position. Symptoms include redness, pain, and open sores, which can progress to deep wounds exposing muscle and bone. Pressure ulcers occur due to reduced blood flow to the affected area, leading to tissue damage. Prevention includes regularly changing positions, using supportive devices, maintaining good nutrition, and keeping the skin clean and dry. Treatment involves relieving pressure, cleaning wounds, and using dressings or medications to promote healing. Advanced cases might require surgical intervention. If you are suffering from a pressure ulcer on your feet or ankles, it is suggested that you schedule an appointment with a podiatrist as soon as possible for care.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with David Mehl, DPM from New York. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions please contact our offices located in Forest Hills, and Brooklyn, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- February 2026
- January 2026
- December 2025
- November 2025
- October 2025
- September 2025
- August 2025
- July 2025
- June 2025
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
